Group Health
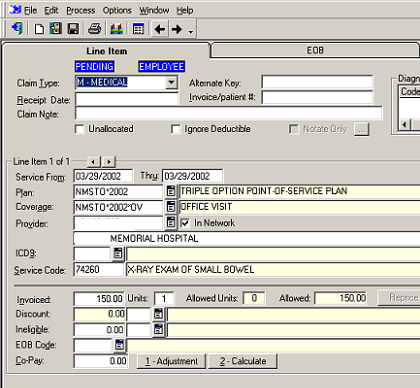
 Important cost containment features include PPO, HMO, UCR, other re-pricing and discounting tables. Flexible plan building.
Important cost containment features include PPO, HMO, UCR, other re-pricing and discounting tables. Flexible plan building.
Integrated with Case Management for pre-certification, disability guidelines and more.
Customizable EOB's and Check formats.
Tiered Benefits based on length of service.
Customizable electronic automated bill adjudication.
Flexible provider and individual EOB's for each claim.
Payments to provider, individual or both. Credits and Recoveries.
In-Network and Out-of-Network calculations.
Extensive Notes and diary system.
Status capabilities such as 'H'old, 'P'end, 'R'elease, and rollback.
Family and individual plan limits, out-of-pocket, co-pay, COB's and carry over accumulators by plan, covered benefit and year.
Customizable alerts, emails and ATS Diaries based on business rules via the ATS/Workflow utility.