Operators with the appropriate authority can
handle any financial operation regarding a claim. The transactions will be
covered in the following order:
- Making General Payments
- Entering Recoveries
- Scheduling Auto Payments
- Voiding Payments
- Changing Reserves
- Editing Batched Payments
- Issuing Credits
- Using the Bill Review Module
If you are in Explore, you can make payments
without actually opening the claim. Simply select the
desired claim and click the General Payments button. The button is also
available if you are already editing a claim and want to make a payment.
Knowing that some bills arrive after a claim
has been closed, the ATS System has a special Stair Step Reserves feature that
may be set so you can make a payment without having to reopen the claim.
The future reserves are always displayed for
your convenience, but the bank account number and the balance in the trust will
not appear if you are creating vouchers. (The number of reserve categories and
their names will depend on how your ATS System has been set up.)
On the upper right side of the screen, you’ll
see a special field that displays the claim number with an ellipsis button to
the right. This field allows you to
enter multiple payments rapidly by saving the payment, typing the next claim
number in this field, entering the next payment and saving. The ellipsis button provides a claim search
function if you don’t have the claim number available.
The example above shows an indemnity payment
that was set up by simply clicking the Ellipsis button next to the amount.
Refer to the fields below for information on this feature. The fields are
described as follows:
|
Field Name |
Description |
|
Pay
Type |
The
payment type is either voucher or check. Note that checks debit the trust
fund (bank account) balance, but vouchers do not. The record shown
above will produce a voucher so the number of the trust fund account and the
balance in the account are not displayed at the bottom of the screen. This information
will appear if you produce checks. |
|
Amount |
The
amount to be paid. A special feature allows you to make an auto indemnity
payment by pressing the Ellipsis button. The program will automatically
display the amount, the employee’s name and address, the default From/Thru dates and “1” in the reserve category field. A
default pay code may also appear. (The defaults are set with the
Administer-Configuration-Application Parameters menu.) If
there is a negative account balance, you may get a "Bank Balance
Insufficient" message depending on a setting entered with the
Administer-Configuration- Module Parameters menu. When this message appears,
the amount will be reset to zero. Another setting may
allow you to enter a batched payment with a negative balance. Attempting to
print a payment or enter a notation will display the message "You may
only batch this payment due to low funds". If you
are using the Stair Step Reserves feature set with the Administer-
Configuration-Application Parameters menu, the reserves will automatically be
increased to cover the payment. |
|
Vendor
Code |
If the
payee is any of the following, enter the code and the program will fill in
the information from the claim. C claimant D dependent (a choice list will
appear) CA claimant’s attorney DA defense attorney P medical provider Otherwise,
enter the vendor code including the asterisk and location or press the
Ellipsis button to select a vendor from the table. |
|
From/Thru
Periods |
The
dates for up to three billing/payment periods may be entered. Pressing the
Ellipsis button next to the amount will display a period based on the Thru
date for the last indemnity payment and whether the Benefit type for the
claim is “TD” or “PD”. By default, these are two week
periods, but the values may be changed with the
Administer-Configuration-Application Parameters menu. If the From/Thru
period is changed for an auto calculated indemnity payment, the program will
display a message explaining how the benefit amount was recalculated and ask
if the amount should be adjusted. When a future date
has been entered, the program will display “Warning: Date entered is greater
than today’s date” on the title bar. Depending on your check printing
schedule, you may need to enter future dates. In that case, ignore the
warning message when it appears. Back
and post-dating payments may be allowed depending on the settings entered
with the Administer-Configuration-Module Parameters menu. Note that it is
very important to be able to back-date a notated payment that was printed on
a prior date. The post-dating feature is also useful since it allows payments
to be entered for printing sometime in the future when you may or may not be
in the office (e.g, on vacation). |
|
Reserve
Cat |
The
code for the reserve category that the payment will be drawn against. If the
payee is a vendor with a default reserve category and pay code, these values
will be displayed on the screen automatically, but they can be modified. |
|
Wage
Continued |
If the
Wage Continued flag is set in the claim, the message “Warning - Wage
Continued” will appear to remind you that an indemnity payment is being made
to an employee who is receiving his or her salary in lieu of worker’s comp
benefits. A
message will also be displayed when auto payments have been scheduled for
that period. Unless the Negative
Reserves value has been set to “Y” with the Administer- Configuration-Module
Parameters menu, the amount to be paid may not be more than the future
reserves for the specified category. If the amount is higher, the program
will read the Stair Step Reserves value set with the Administer-
Configuration-Application Parameters menu. If the value is “N”, you will be
given an opportunity to edit the reserves and increase the amount so the
payment may be issued. For example, “Futures insufficient by 286.00. (Use the
Change Reserves icon on the tool bar.” If Stair Step
Reserves contains an “A”, the incurred amount will be automatically increased
by the amount of the payment. A value of “C” will increase the reserves for
closed claims only. In both cases, the future reserves will still be zero
after making the payment. Refer
to the Editing Reserves section in this chapter for more information on this
process. |
|
Payment
Code |
The
payment or cost center code for the specified reserve category. Default codes
for auto TD or PD indemnity payments may be set with the Administer-
Configuration-Application Parameters menu. |
|
OSHA
Days |
When making a payment
to the employee from reserve category 1 or 3 (indemnity or rehab), the
program will check the contents of the Grouper field in the specified Payment
Code. If this value contains “TD”, then the From/Thru
days are used to calculate the OSHA Days based on a calendar week. This value
will be displayed on the screen and added to the existing values in the claim
record. There
will be times when an employee performs another job or the same job with
restrictions due to an injury or illness. If the job pays less than the
usual, the employee should get a comp payment to make up the difference. In
that case, it is very important that the temporary disability payment is made
with a pay code that contains I08 (wage loss) in the report category so the
days in the From/Thru period will be ignored when
reporting to OSHA. If this feature is not used, the days would be counted as
lost time when the employee is really at work. |
|
Note |
An
optional note or memo to be displayed on the check/voucher. |
|
Status |
There
are three choices: 1.
Batch the payment record so that it can be printed later
or exported with the Accounting Interface module. 2.
Notate payments that were issued without using the ATS
System. For example, suppose a check is lost. After voiding the original
payment, enter a notated payment with the same date. 3.
Click the Print button if you want to print the payment
immediately. |
|
Form
Number Process
Date |
When
the Status is Print or Notate, the program will make these fields available
and fill in the form number and current date which can be changed if
necessary. This is a handy
feature when the original payment was incorrect (e.g. has the wrong reserve
category) and has to be voided. You can’t batch
another payment because the check has already been cashed. In this case, you
will need to enter a notated payment Note
that the next check number is stored in the bank information entered with the
Trust Fund menu while the voucher number is in the client’s record. |
|
Due
Date |
The Due
Date field is available when the payment is to be batched. If there is no
specific date, leave the field empty so the payment will be included the next
time a batch is printed. Back
and post-dating payments may be allowed depending on the settings entered
with the Administer-Configuration-Module Parameters menu. Since the Print
Batch program asks for a due date, the post-dating feature allows you to
enter payments to be printed in the future. It is also important to be able
to back- date a notated payment that was printed on a prior date. |
|
Separate
Handling |
If
the Separate Handling box is checked, the payment will not be combined with
other payments to the same vendor. Checking this box also allows you to
inform the accounting department (when the Handle Return File option in the
Accounting Interface is used) that the check should be sent back to claims
for special handling before it is mailed. |
|
EDI
Late Reason |
Each
state requires that the initial indemnity payment is issued a specific number
of days after the date of injury. If this payment will be transmitted to the
state via EDI, then select a code to indicate why the payment is late.
Omitting the code may cause the state to reject the transaction. |
|
Invoice
Number |
The
invoice or reference number being paid, if any. |
At this point, the program will search for
possible duplicate payments for the same payee, reserve category, pay code and
from date. If one is found, the program will display all the details on the
other payment(s) so you can decide whether you should click Continue and save
the payment. Clicking Cancel will leave you in the payment screen without
saving the record the payment is over this amount, the program will display
“Over check limit. Record will be pended.” The payment will be pended until
someone with a higher limit releases it (to batch) with the Process- Edit Batch
menu.
In states such as Florida and South Carolina,
the MMI Date in the claim determines whether a $10 copayment can be applied to
a medical payment. A message will appear if the date has been reached. Click Yes to apply the $10. The No button will return to
the payment program. When you Save the record, the program will clear the
screen except for the payee. At this point, you can enter another payment to
the same or a different payee or exit the program.
The AutoPay module is included with the
standard ATS System so you may schedule payments to be made on a regular,
ongoing basis. This feature is available from the menu from within a claim or
from the Selected Claims list screen after selecting a claim.
The program displays the following screen. .
Depending on how the claim has been set up, the
following buttons may be used.
|
Button |
Function |
|
Edit |
Displays
the selected payment record for viewing and/or editing purposes. If the list
is empty, this button will be disabled. |
|
New |
Displays
a blank form so a new record may be entered. |
|
Auto
Setup |
Sets
up a new payment schedule automatically. This button will be disabled if
there is a Start TD or Start PD Date in the claim. |
|
Close |
Exits
to wherever you started, either the claim or the Selected Claim menu. |
There are two ways of scheduling new payments.
Each method will be covered in this section.
Using the Auto Setup of Compensation Button
The Auto Setup button is available for setting up the benefit
period. It will be enabled for indemnity claims that have a specific Benefit
Rate, but no benefit payments (i.e. the Start TD and Start PD Date fields are
both empty).
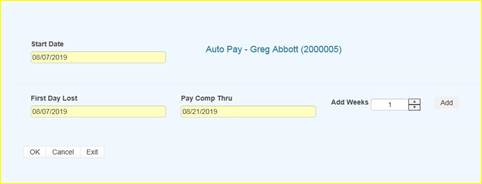
Selecting the button will prompt for the
compensation period. The First Day Lost will be displayed if the date exists in
the claim record. Enter the date when the period will end. It can always be
changed later. If you don’t know the exact date, add the number of weeks to be
paid and click the Pay Comp Thru field to update the ending date.
Click OK and the program will set up the
payment schedule as shown in the following example.
In addition to the information found in the
claim record, the program will search the various tables to find the default
values for the Pay Code, State Days, and Waiting Period when the Auto Setup of
Compensation feature is used. (All of the fields will be covered next.)
If the program finds all the required
information and the Pay Day value for the employer is set to something besides
any day, then the only thing left to do is save the record. Otherwise, the date
for the Next Check must be entered before the record can be saved.
Using the New Button to Schedule Payments
If you use the New button,
normally the information on the form will have to be entered manually. The
fields are described as follows:
|
Field Name |
Description |
|
Record
# |
The
default is “1” for the first payment schedule. Enter “2” to indicate a 2nd
one. A
total of nine records may exist at any one time. Records no longer appear on
the list after the last payment has been made. |
|
PMT
Type |
The
payment type
is either checks
or vouchers. If necessary, a
system administrator may change the default value. |
|
Payee
ID |
The
payee’s social security or federal ID number. Enter "C" if the
payee is the claimant, "D" for a dependent receiving alimony or
child support, or press the Ellipsis button for a
list of vendors. If
this is a fatality case, we recommend that you enter the individual who will
receive the death benefits as a dependent to make it easier to schedule
payments. |
|
Payee |
The
name of the payee will be filled in automatically after reading the social
security number or vendor code in the previous field. |
|
2nd
Payee |
The
name of a second payee if any. For example, if the employee's check needs to
go to a legal firm for disbursement, the c/o name should be entered here. |
|
Address,
City, State, Zip, Phone |
The
address and phone information will be filled in automatically after reading
the record with the specified social security or federal ID number. |
|
RSV
Cat |
The
reserve category to be used. The Auto Setup feature will enter “Indemnity” by
default. Press the Ellipsis button for a list of other categories that are
available on your system. |
|
Pay
Code |
The
payment or cost center code. Press the Ellipsis Button for a list of codes
that are available for the specified reserve category. If
the Auto Setup button is used, the program will use the Benefit Type code
specified in the claim record to look for the default code set up with the
Administer-Configure-Application Parameters menu. |
|
Rate |
The
employee’s benefit rate. If an amount has been entered in the claim record,
it will be displayed here automatically. (A benefit rate must have been
entered in the claim in order to use the Auto Setup feature.) |
|
Work
Comp From |
When
the Auto Setup of Compensation button is used, the program will calculate the
starting date based on the First Day Lost and the days in the state's waiting
period, otherwise it must be entered manually. In either case, the From Date
will be adjusted as payments are made. |
|
Work
Comp Thru |
The
day benefits should end. The program that batches the payments will generate
"Next to Last Payment" and "Last Payment" diaries to warn
the adjuster that the claim should be reviewed. This date may be modified if the payment
period needs to be shortened or extended. |
|
Wait
Period From/Thru |
When
the Auto Setup of Compensation button is used, the program automatically
calculates the From and Thru dates based on the Waiting Period and Before
Paid values in the record for the claim's state of jurisdiction. This
feature will not work correctly if the values in the state's record are
incorrect. If for some reason, you do not want the program to calculate the
waiting period payment, zero out the values for the state. |
|
Pay
Period |
The
Auto Setup feature will automatically enter “B” (bi-weekly) as the Pay
Period. Other
valid entries are “W” (weekly) and “M” (monthly). |
|
Benefit
Type |
The
benefit type from the claim record, either “TD” (temporary disability), “PD”
(permanent disability), or “VR” (vocational rehabilitation). |
|
PMT
Periods |
The
total number of payments to be made will be calculated after you have entered
the pay period and from/thru dates. This value can not
be modified. It will be updated automatically as payments are made. |
|
Original
From |
The
Comp Period From Date will be updated as payments
are made, but the original date is displayed here for your information. |
|
Next
Check |
The
date of the next payment. This date will appear as the first Batch On date on
the list of future payments. (See below for details.) |
|
Prior
Check |
The
date of the last payment that was batched. |
When the record is saved, the program will
check the claim to verify that there are sufficient
reserves to make the payments. If there aren’t, you will be prompted to
increase the reserves accordingly.
AutoPay creates the payment schedule and
displays it on the screen as it saves the record. This particular
example was created to batch the payments after the pay period (AutoPay
Mode set to A) and the employer’s Pay Day set to any day. (Refer to the Setup
Procedure in a later section.) The Next Check date is used as the first Batch
On date. This is the most typical configuration.
Note the first payment on the list is for the
waiting period. In the state of jurisdiction for the claim, there is a 14 day period before those days can be paid.
Typically, the Comp Thru Date does not fall at
the end of a pay period so the last payment is only for a few days. When that
happens, the program will check the Scheduled Hours in the claim record.
If there are no Scheduled Hours, AutoPay
assumes that the individual works a regular week and calculates the payment
accordingly. But, suppose the employee works Monday and Wednesday through
Saturday. (Work days are those which contain a value
in the Total field on the Scheduled Hours dialog.) If the Thru Date falls on a
Wednesday, the program will know that the employee does not work on Tuesday and
only pay for two lost days.
The program that batches the auto payments will
generate a diary to the adjuster when the next to the last and the last
payments are batched.
The Autobat program
must be run to batch payments according to their Batch On date. AUTO will be
stored as the user who processed the transaction. Although the reserves must be
sufficient to schedule the payments, the reserves may
have been used up since then.
Auto payments will always be batched because of
a possible late penalty. When the reserves are insufficient, the program checks
the Stair Step Reserves value entered with the Application Parameters. If it is either "Closed" or
"All", the reserves will be automatically increased to cover the
payment. Unless Negative Reserves has been set to “N”, the futures will become
negative. In any case, a diary will be sent to the adjuster.
Auto Batch logs may be viewed with the Image
Files menu. When appropriate, "Next to Last Payment" and "Last
Payment" entries will appear along with a diary telling the adjuster to
review the claim.
The number of OSHA Days in the claim is updated
as payments are batched against reserve categories 1 and 3 (indemnity and
rehab) for pay codes with “TD” in the Grouper field. This number is based on a
calendar week.
The system administrator must set up AutoPay so payment schedules are created to meet your particular
needs. When the record is saved, the program will check the Pay Day and AutoPay
Mode values as defined below.
|
Item |
Set In |
Value |
|
Pay
Day |
Employer’s
record |
Sunday
thru Saturday or Any Day |
|
AutoPay
Mode |
Application
Parameters |
Standard
(sets the first Print Date to the first Pay Day at the end of the pay period) After
(sets the first Print Date to the first pay day after the pay period ends) |
When the
Auto Setup of
Compensation feature is used and Pay Day is set to a specific day of the week,
the program will ignore the Next Check date, if one exists, and use the AutoPay
Mode to calculate it and the subsequent Print Dates (displayed with the List
option). Changing the Next Check date will have no effect.
The Reserve
Change button
will display the following dialog so the reserves for an open claim may be
changed depending on the permissions granted in your user’s profile. This
dialog also appears when the reserves must be increased in order to enter a
payment.
Before the modified reserves can be saved, a
Reserve Change reason must be selected using the drop-downs
on the right. These changes may be viewed later with the History module.
There are two types of reserve limits that may
be set in the ATS Security System: a Cumulative Limit
which is the total incurred entered per user that cannot be exceeded and a One
Time Limit which is the amount that may be entered during a session. (A session
ends after exiting the program.)
These limits may apply to the total reserves or
to individual reserve categories. For example, suppose the One Time Limit is
set to 25,000 and the Cumulative Limit is 50,000. Depending on the current
amount in the specified category, the change may or may not be allowed. Note
that the Cumulative Limit examples assume that prior changes to the incurred
were made by the same user.
One Time Limit=25,000 Cumulative Limit=50,000
Incurred in Claim Reserve
Change Allowed?
Example 1 15,000 25,000 YES
Example 2 35,000 25,000 NO
Example 3 45,000 10,000 NO
It is important to note that when both the
limits are zero or null, there is no limitation on the changes that may be
made. If the One Time Limit is set to 25,000 and the Cumulative Limit is zero,
the user may increase the reserves up to $25,000 a session regardless of the
current amount in the claim.
One Time Limit=25,000 Cumulative Limit=0
Incurred in Claim Reserve
Change Allowed?
Example 1 15,000 25,000 YES
Example 2 35,000 25,000 YES
Example 3 35,000 35,000 NO
Conversely, if the One Time Limit is set to
zero and the Cumulative Limit is 50,000, the reserves may be increased by any
amount until a total of $50,000.
One Time Limit=0 Cumulative Limit=50,000
Incurred in Claim Reserve
Change Allowed?
Example 1 15,000 25,000 YES
Example 2 35,000 15,000 YES
Example 3 5,000 50,000 NO
The program will automatically update the
future reserves and display the new totals as the incurred values are modified.
There may be times when you need to issue a
credit against a specific claim. The credit might be for a particular
payment when there was an overpayment. A credit may also be issued when
there has been money recovered and the amount should be subtracted from the
amount paid. In that case, there would be no prior payment involved.
Regardless, if the claim is closed and the futures are zero, they will remain
zero after the transaction has been made. Each of these type
of credits will be covered in this section.
Select the Payment History button if you need
to issue a credit for all or a part of a specific payment. The following screen
will appear with a list of the payments that have been made. The list may
include some existing credits where the form number ends with *R and a number.
Scroll through the list until you find the
payment you want. Then, select the
payment and click the Credit button. The program will display the Credit
screen along with the data from the original payment. Note the Status field. A
warning message will appear if you attempt to credit a payment that has been
voided.
The cursor will be positioned in the Credit
Date field so that you can modify the following items. Save the record to
complete the transaction.
|
Field Name |
Description |
|
Credit
Date - Time |
The
current date and time appear by default. |
|
Amount |
The
amount to credit may not exceed the amount of the original payment. If a
credit has already been applied, it will be subtracted from this value. |
|
Note |
The
note or
memo that appeared
on the original
payment is displayed. It may be
modified to indicate the reason for the credit. |
This option allows you to issue a credit for a
claim when there is no particular payment involved
(e.g. the credit applies to a group of payments). This feature should also be
used when the money recovered on a claim must be deducted from the amount paid.
In this case, the amount could not be entered as a recovery since these are
tracked separately in the ATS System.
After selecting the desired claim, pick the Credit (no check) button. The program will display
the same form used to issue standard credits, but the information has to be
entered manually since there is no payment record..
The fields on the form are described as
follows:
|
Field Name |
Description |
|
Vendor
Code |
If the payee is any of
the following, enter the code and the vendor code, name, and address will be
filled in with the information in the claim record.
If
the payee is someone else, press the Ellipsis button to search for the
vendor. |
|
Reserve
Cat |
The
code for the reserve category to be credited. |
|
Amount
PTD |
As
soon as the reserve category has been specified, the total amount paid for
that category will be displayed. |
|
Payment
Type |
The
type is either check or voucher. |
|
Credit
Date/Time |
Normally,
this data is not changed. |
|
Reason |
A
note explaining why the credit was issued. |
|
Credit
Amount |
The
amount to be credited may not exceed the amount paid. |
In the ATS System, recoveries are tracked
separately from payments, credits, and voids. The amount paid will not be
adjusted. Use the Credit menu when the money received must be deducted from the
amount paid against the claim.
The fields to be entered on the form are
described as follows:
|
Field Name |
Description |
|
Recovery
Amount |
The
amount recovered. A warning will be displayed if this amount is greater than
the amount paid. |
|
Vendor
Code |
The
code for the vendor making the payment. Press the Ellipsis button to search
the vendor records or enter “C” to display the Claimant’s information or
"S" to display the Recovery (Subro) Party
from the claim. In the latter case, no vendor code will appear because there
is none in the claim. |
|
Invoice
No./Date |
The
invoice or reference number and date. (optional) From/Thru The range of dates in
the period. (optional) |
|
Reserve
Category |
The
code for the category from which the recovery will be made. |
|
Recovery
Type |
The
code indicating the type of recovery is normally a required field. |
|
Note |
An
optional note regarding the recovery. |
|
Recovery
Date - Time |
The
current date and time may be modified if necessary. |
|
Update
Bank |
A
check will update the bank balance (i.e. the client’s trust fund). This value
has no effect if you use the ATS System to issue vouchers, not checks. |
Menu options are available so that you may void
a payment or recovery. Typically, that is necessary when a transaction was
entered incorrectly.
Whether the payment was entered for the wrong
reserve category and pay code or it was lost in the mail, the original
transaction should be voided and re-entered.. This is
done by selecting the History button . The following
screen will appear with a list of the payments that have been made.
Scroll through the list until you find the
payment you want. Then, select the
payment and click the Void button. The program will display the Void
screen along with the data from the original payment.
The following screen is used to void payments.
The only fields that may be edited are the Void Date, Reason, and the Type.
Simply save the record to void the payment.
If the claim is closed and the futures are zero, they will remain zero
after the transaction has been voided.
Note:
1. Voiding a benefit payment may affect the Start
TD or Start PD dates in the claim. If the first payment is voided, the new
starting date will be the From Date in the second payment.
2. If the claim is closed and the futures are
zero, they will remain zero after the transaction has been voided.
Suppose you receive money on a claim and enter
it as a recovery before realizing it should have been a credit so the amount
would have been deducted from the paid. In that case, you will need to void the
original transaction by selecting the Recovery History
button.
The following screen will appear with a list of
the recoveries that have been made.
Highlight the record to be voided click the
Void button. The date, the reason for voiding the transaction, and a code
indicating the type of void are the only items that can be entered. To void the
recovery, simply save the record. If the bank (trust fund) was updated when the
original recovery was made, a message will appear to let you that the balance
has been adjusted.
All payments that are entered with a status of
“B” are batched for future processing. At any time, these batched payments may
be reviewed, approved, posted, deleted and/or released (when pended) by anyone
with the proper access level.
Use the Process-Batched Payments menu and click
Process to view all the payments.
Use the Previous and Next buttons to page
through the list. The columns contain the following information.
|
Column |
Contents |
|
Type |
The
type of payment where C = check and V = voucher |
|
Status |
“A”
if the Approve feature is used, otherwise empty. |
|
Entry |
The
code for the user who entered the payment or AUTO if the system batched the
reoccurring payment. |
|
Amount |
The
amount of the payment |
|
Payee |
The
name of the payee |
|
From/Thru |
The
dates in the billing period |
|
Due |
The
date the payment is to be issued |
|
Desc |
The
pay code |
|
Transaction |
The
claim number followed by an asterisk and the number of the payment issued for
the claim |
|
Voucher |
The
number assigned
when the item
has been exported
with the Accounting Interface
module |
|
Entry
Date |
The
date the payment was batched |
The Edit Batch utility has a wide variety of
features as evidenced by the number of buttons and check/edit boxes that appear
on the form. Each of the features, including those available from the menu,
will be covered in the following sections.
There are two buttons that may be used to
process batched (the default) or pended payments which were entered for more
than the operator’s check writing limit.
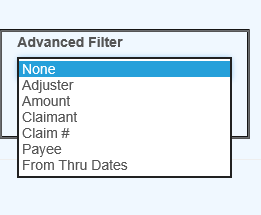
The following filters are available to select a
specific group of batched payments.
The ATS System has a Pre-Approve feature that
may be used to require the approval of payments before they can be printed.
If the Pre-Approve flag has been set using the
Module Parameters screen, these filters will be enabled so that all payments
that are not approved will be listed when the Process button is clicked. Remove
the check in the Not box to get a list of approved payments. (Approved payments
will have an "A" in the Status column.)
By default, all the payments that have not been
exported using the Accounting Interface will be listed. Remove the check in the
Not box to get a list of exported payments that have a number in the Voucher
column.
When the Region feature has been implemented,
this filter may be used to display a list of payments for claims in a specific
region. An operator may only view payments for a particular
region if one is specified in the operator's record and the Region View
is turned on.
By default, the payments for all the claims
that meet the other criteria (filters) will be listed. When this is a long
list, it may be difficult to find a payment for a specific claim. In that case,
click the Claims ellipsis button to display the Select Claim screen. Pick a
claim and only those payments will appear on the list.
The Payment program allows you to specify a Due
Date for each batched payment. By default, this field is empty so this filter
will have no effect.
Depending on the settings entered using the
Module Parameters screen, post-dating payments may be allowed. In that case,
the Due Date filter may be used to display payments with dates either on or
before the date specified (in the filter) or blank.
A variety of buttons are available so you can perform
the following functions.
If the Pre-Approve flag has been set to
"Y" using the Module Parameters screen, the Approve button will be enabled so batched payments can
be approved by an operator with the authority to print checks. Otherwise, this
button will be disabled (grayed out) since this step is not required. When this
feature is used, approved payments will have an "A" in the Status
column.
Any payment may be deleted from batch by an
operator with Delete permission. Simply highlight the desired item and click
the Delete button. The program will ask if you want to
perform the operation. To continue, click the Yes button.
The program will remove all references to the batched payment from the system
and adjust the reserves/paid amounts for the claim.
When a check has been made out by hand or
printed with a foreign system, an operator with Print Payments permission
should use the Post button to post the payment to the check
history table. The date and form number may be changed if necessary.
The next voucher number is found in the
client’s record, whereas check numbers are stored in the information for the
bank account.
Use Pend mode to view any payments that were
entered for an amount over the operator’s check writing limit. Select one of
the payments. If your check writing limit is higher than the amount of the
payment, the Release button will be available to place it in Batch
mode.
Use the View
button to view all of the information on a specific
payment. Notice the Browse button in the Payee group. Suppose that a
payment had issued to the wrong vendor. This button may be used to display the
Select Vendor dialog and pick the correct vendor without having to void the
payment and enter a new one. After making a change, click the Process button again to update the Payee name on the
list.
The Edit Batch Report
button may be used to produce a wide variety of reports with the currently
listed payments. Clicking the button will display the specification screen with
all of the default values as shown below. Check the
Page Eject box if you want a new page to be used when the value being sorted by
changes.
The report specifications are as follows:
|
Field |
Contents |
|
Sort
By |
Payments
may be sorted by Adjuster (the default), Claimant, Reserve Category/ Pay
Code, ATS Claim Number, Alternate Claim Number, or Region/Level 1. |
|
Mode |
Batched
or Pending payments. |
|
Checks |
A
check will display only checks on the report. |
|
Vouchers |
A
check will display only vouchers on the report. |
|
(Un)
Approves |
If
the Pre-Approve feature is used, a check will indicate which payments should
be included. |
|
(Not)
Exported |
A
check will either include the payments that have been exported (for printing)
or not. |
|
Claim
Number |
By
default, the wildcard % is used to include all claims. Click the ellipsis
button to select a particular one. |
|
Region |
By
default, payments for all regions will be included. |
|
Level
1 |
By
default, payments for all levels will be included. |
|
Page
Eject |
A
check will cause a page eject each time the Sort By
value changes. |
When you have finished entering the
specifications, click the Print
Preview button to
load the report into the ATS Print Previewer where it may be reviewed and/or
printed.
Each year, medical costs continue to skyrocket.
Instead of simply paying the full amount on every invoice, use the Medical Fee
module, an optional, add-on product designed to lower your medical costs. Each
line item on the invoice is calculated and either accepted or overridden based
on the state’s fee schedule, the DOL’s OWCP schedule, and/or the Usual and
Customary Reimbursement (UCR) value. A vendor’s custom fee schedule may also be
used.
This module has also automated the printing of
Explanation of Benefits to the medical providers. The UCR module is an optional
feature and not part of the standard ATS/Comp Medical Fee product.
Bundling and unbundling is another optional
feature that is available. The data to implement any of these features is
available from a third party.
1. By
default, the program will check to see if the specified vendor has an HMO/PPO
with Valid From/Thru dates that cover the From date in
the payment record. If so, it will look in the HMO/ PPO’s record for the rate
table to be used.
When a rate table is not specified (or found),
the program will use the vendor’s State to see if the Schedule flag for that
state has been set with the Maintain-State Codes menu.
If the vendor’s State field is empty or the
state has no fee schedule, a message will appear indicating that it will use
the Fee State Code set with the Administer-Configuration-Module Parameters menu
to calculate the amount for the line items to be paid on the invoice.
2. If
UCR percentiles are to be used, they should be stored by state with the Medical
Fee- UCR Percentile menu. By default, the program will detect that a percentile
exists for the vendor’s state and use the UCR value to calculate the amounts,
based on the zip code,
for the line items ignoring the $ per Unit value in the fee
schedule.
3. If
the Override State flag has been set with the Module Parameters menu, the
program will calculate the amount of the line item using both
of the above methods and display whichever amount is lower.
The bill review process is quick and easy. The Bill Review button will display a data entry screen with
two pages, the first of which is used to enter general information on the
payment as shown below.
|
Field Name |
Description |
|
Payment
Type |
The
type of payment, either check or voucher. |
|
Invoice |
The
number of the invoice that is being paid. |
|
Invoice
Date |
The
date of the invoice. |
|
Received |
The
date the department received the invoice may be entered for accounting
purposes |
|
Status |
The
status of the payment; either batch to be printed later, print when the
record is saved or notation only, which writes the payment record to the
check history file with a specified form number and processed date without
printing it first. |
|
Payment
Code |
The
code for the type of payment. |
|
Payment
Note |
A
note to be displayed on the check or voucher. |
|
Vendor
Code |
Enter
“C” if the payee is the claimant or press the Ellipsis button to select an
active vendor. |
|
Payee |
Making a selection will display the
name and address from the vendor’s record. |
Clicking the Line Items
button will display the page shown below.
The fields on this form are described as
follows:
|
Field Name |
Description |
|
Amount |
The
amount on the invoice. The total amount that will be paid for the line
item(s) is displayed in the Payable field. The program will display a message
and adjust the amount for the line item or the amount payable if either is
greater than the invoiced amount. |
|
Service
Zip |
By
default, the vendor’s zip will be displayed as the zip code where the service
was performed. This zip code will not only determine which fee schedule is
used, but also the tax rate if tax is to be applied as in New Mexico. |
|
ICD-9 |
The
ICD-9 code(s) from the invoice. Up to four codes may be entered. |
|
Inpatient |
A
check indicates that the employee has been admitted in a facility and treated
as an inpatient. |
|
Item |
The
number of the line item. Use the arrow keys to enter another item or review a
previous one listed in the grid below. |
|
From/Thru |
The
starting and ending date of the billing period. (The default ending date is
the same as the From Date.) These dates will determine which particular fee schedule to use. (It must be after the open
date on the claim.) For
your convenience, the previous From/Thru dates will
be displayed as you enter new line items. |
|
ICD-9 |
A
number to specify which ICD-9 code applies to the specified CPT code for the
line item. |
|
Invoiced
CPT Code |
The CPT
code for the item. Normally, this must be a valid code (in the fee schedule)
in order to continue. The exception is “00000”, which may be used to enter a
miscellaneous item that is not found in any fee schedule. Note
that the professional component or technical unit value may be used instead
of the maximum reimbursable by entering the CPT code followed by either
"-26" or “-27” respectively (e.g. 00100-26). |
|
CPT
Code |
If
the UCR module is in use, the vendor’s zip code will be used to determine the
appropriate region. |
|
Description |
The
description of the procedure. |
|
Modifiers |
Up
to three modifiers may be applied to the CPT code. For example, the following
modifiers may be applied to CPT 00100. |
|
Specialty |
When
there is a specialty associated with the CPT code, it may be selected from a
list of choices by clicking the Ellipsis button. |
|
Qty |
The
number of units billed for this line item. Unit Amount The amount billed per unit is optional. |
|
Amount |
The
amount billed for the procedure. If the amount per unit has been specified,
the program will multiply it by the quantity when the Qty is greater than one
and the CPT code begins with 1 or higher (anesthesia units are billed
differently). When
the following situation occurs, the invoiced amount will be set to zero. The
values from the preceding Invoiced fields will appear as soon as the Amount
is entered. |
|
Accepted
Amount |
The
Maximum Reimburseable Amount (MRA) is displayed if
it is less than the amount invoiced, otherwise the MRA will appear. As the
amount of each line item is accepted, the total value in the Payable field
will be incremented. Note
that if the Bundling/Unbundling feature is in use, the program will check for
major or comprehensive procedures that consist of a number
of individual procedures. For example, the CPT code 31505 (larynoscopy diagnostic) consists of many other
procedures, one of which is 36000 (microsurgery add-on). If both are on the
same bill, the program will detect that the "code 36000 is part of the
comprehensive procedure code 31505" and enter ZERO in the accepted
amount for line 36000. The program will also look for mutually exclusive procedures
(e.g. 27177 and 11010) that are not allowed on the same bill. |
|
Override |
An
override code to explain why the amount to be paid is different than the
amount billed. Press the Ellipsis button for the user-defined choices entered
with the Tables-Medical Fee menu. |
|
Futures |
The
amount available in the claim’s (future) medical reserves. See below for
details when the amount is insufficient to cover the payment. |
|
Payable |
As
line items
are entered and
accepted, the program
will adjust this
value accordingly. When the record is saved, this amount will be used
to update the paid to date and future reserves in the claim. |
|
Rate
Table |
The
program will display the name of the fee schedule table in use. |
If you are in the Override field and want to
enter another line item, press <Page Down> to increment the Line Number by one and move the cursor to the
next From field. By default, the previous From/ Thru
dates will be displayed for your convenience.
After all the line items have been entered,
save the record. The program will verify that the future medical reserves will
cover the payment. If the futures are not enough, the program will check the
Negative Reserves value set with the Module Parameters menu.
If the Negative Reserves value is
"Y", the entry is allowed and the future reserves in the claim will
become negative. If the value is "N", the program will check the
Stair Step Reserves value that was set using the Application Parameters screen.
If the Stair Step Reserves value is “A”, the
incurred amount in the claim will automatically be increased to cover the
payment. Otherwise, the Edit Reserves dialog may be used to increase the
reserves. (All changes depend on the operator's reserve limit.) Clicking Close without making a change will decrease the
amount to equal the future reserves.
At this point, the payment will be batched,
printed, or manually posted to history depending on how the Status field is
set.
Note that the payment will be pended if it is
over the operator’s check writing limit. (Pended payments must be released
using the File menu in the Batched Payments section of the Process module.)
After the record is saved, you will be asked if
you want to input another payment for this claim. If you click Yes, the form will be cleared so you can start
again. Otherwise, you will be returned to the main menu.
The Bundling and
Unbundling Feature
When this optional feature is in use, the
program will check for mutually exclusive procedures (e.g. 27177 and 11010)
that are not allowed on the same bill. It will also look for major or
comprehensive procedures that consist of a number of
individual components or procedures. For example, the CPT code 31505 (larynoscopy diagnostic) consists of many other procedures,
one of which is 36000 (microsurgery add-on). If both are on the same bill, the
program will detect that the "code 36000 is part of the comprehensive
procedure code 31505" and enter ZERO in the accepted amount for line 36000.
The ATS system supports multiple fee schedules;
federal (DOL), state, and the usual and customary reimbursement (UCR) schedule.
In that case, the program will display the amounts in the different schedules
so the user can make a selection.
Discounts and/or custom fee schedules can also
be setup for specific vendors. (Without this ability to use custom schedules,
invoices for vendors that use their own service codes could not be reviewed.)
After custom schedules have been setup, their use is transparent during data
entry unless the code on the invoice is found in multiple schedules.
If you would like to use this feature, please
contact ATS support as the procedure is beyond the scope of this manual.
Printing the
Explanation of Benefits
The Explanation of Benefits (EOB) is normally
printed at the same time as the payment. A special menu option is provided for
those clients who export their payments to be printed by a foreign system
and/or want to print them again later.
An option on the Financial menu may be used to
print the EOBs any time after the check or voucher payments have been printed
(not while they are still batched). When the report screen appears, enter the
specifications to meet your requirements.
|
Field Name |
Description |
|
Provider
Code |
A
specific provider (vendor) code. Leave this field empty to include every
provider that received a payment within the specified range of dates. |
|
Display
By |
The
EOBs will be sorted by provider code and then by either the claimant’s name
(the default) or the claim number. |
|
Starting
Date |
The
first payment date to be selected. By default, this is the date that was used
the last time the forms were produced. |
|
Ending
Date |
The
date of the last payments to be selected. |
An example of the standard EOB has been
included below.
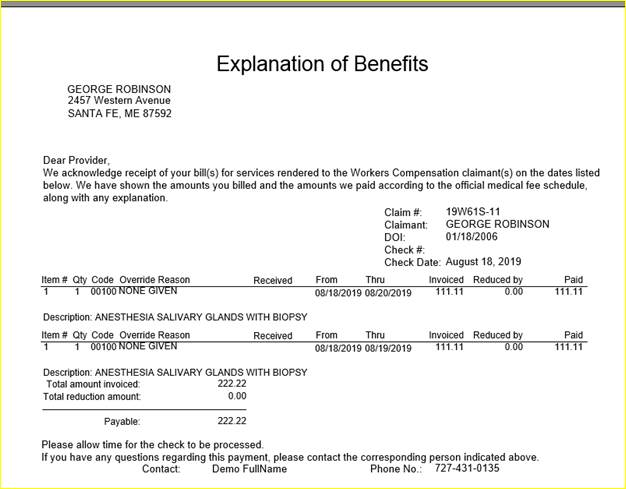
Figure 6‑3: Sample Explanation of Benefits
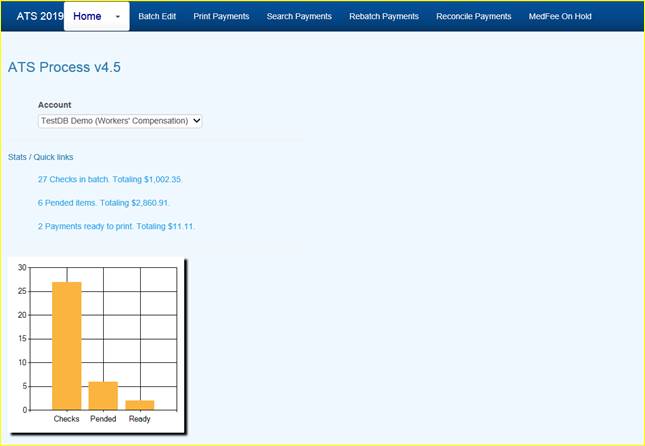
All payments that are entered with a status of
“B” are batched for future processing. At any time, these batched payments may
be reviewed, approved, posted, deleted and/or released (when pended) by anyone
with the proper access level.
Use the Batched Payments menu and click the Process button to view all the payments.
Use the Previous and
Next buttons to page through the list. The columns
contain the following information.
|
Column |
Contents |
|
Type |
The
type of payment where C = check and V = voucher |
|
Status |
“A”
if the Approve feature is used, otherwise empty. |
|
Entry |
The
code for the user who entered the payment or AUTO if the system batched the
reoccurring payment. |
|
Amount |
The
amount of the payment |
|
Payee |
The
name of the payee |
|
From/Thru |
The
dates in the billing period |
|
Due |
The
date the payment is to be issued |
|
Desc |
The
pay code |
|
Transaction |
The
claim number followed by an asterisk and the number of the payment issued for
the claim |
|
Voucher |
The
number assigned
when the item
has been exported
with the Accounting Interface
module |
|
Entry
Date |
The
date the payment was batched |
The Edit Batch utility has a wide variety of
features as evidenced by the number of buttons and check/edit boxes that appear
on the form. Each of the features, including those available from the menu,
will be covered in the following sections.
There are two buttons that may be used to
process batched (the default) or pended payments which were entered for more
than the operator’s check writing limit.
The following filters are available to select a
specific group of batched payments.
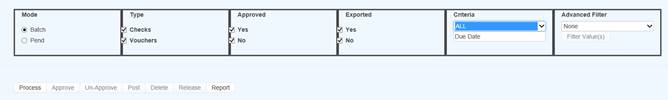
Figure 6‑5: Batch Mode Filters
The ATS System has a Pre-Approve feature that
may be used to require the approval of payments before they can be printed.
If the Pre-Approve flag has been set in Module
Parameters, these filters will be enabled so that all payments that are not
approved will be listed when the Process button is clicked. Remove the check in
the Not box to get a list of approved payments. (Approved payments will have an
"A" in the Status column.)
By default, all the payments that have not been
exported using the Accounting Interface will be listed. Remove the check in the
Not box to get a list of exported payments that have a number in the Voucher
column.
When the Region feature has been implemented,
this filter may be used to display a list of payments for claims in a specific
region. An operator may only view payments for a particular
region if one is specified in the operator's record and the Region View
is turned on.
Also available is the due-date filter.
By default, the payments for all the claims
that meet the other criteria (filters) will be listed. When this is a long
list, it may be difficult to find a payment for a specific claim. In that case,
click the Claims ellipsis button to display the Select Claim screen. Pick a
claim and only those payments will appear on the list.
![]()
A variety of buttons are available so you can
perform the following functions.
Approve/Un-Approve
If the Pre-Approve flag has been set to
"Y" with Module Parameters, these buttons will be enabled so batched
payments can be approved by an operator with the authority to print checks.
Otherwise, this button will be disabled (grayed out) since this step is not
required. When this feature is used, approved payments will have an
"A" in the Status column.
Any payment may be deleted from batch by an
operator with Delete permission. Simply highlight the desired item and click
the Delete button. The program will ask if you want to
perform the operation. To continue, click Yes. The
program will remove all references to the batched payment from the system and
adjust the reserves/paid amounts for the claim.
When a check has been made out by hand or
printed with a foreign system, an operator with Print Payments permission
should use the Post button to post the payment to the check
history table. The date and form number may be changed if necessary.
The next voucher number is found in the
client’s record, whereas check numbers are stored in the information for the
bank account.
Use Pend mode to view any payments that were
entered for an amount over the operator’s check writing limit. Select one of
the payments. If your check writing limit is higher than the amount of the
payment, the Release button will be available to place it in Batch
mode.
 View
Button(s) on the grid
View
Button(s) on the grid
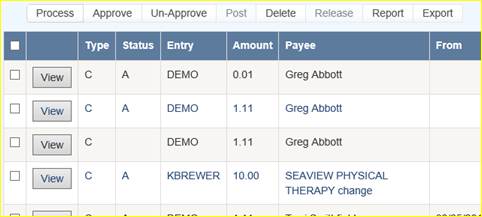
Use the View
button to view all of the information on a specific
payment. With proper authority information within the batched payment can be
modified.
The Report button may be used to produce a wide variety
of reports with the currently listed payments.
The Export button will export the grid to a Microsoft
Excel type format.
This feature is used to search printed items
that may need to be reprinted due to a print job error or a mistake on a check
or checks.
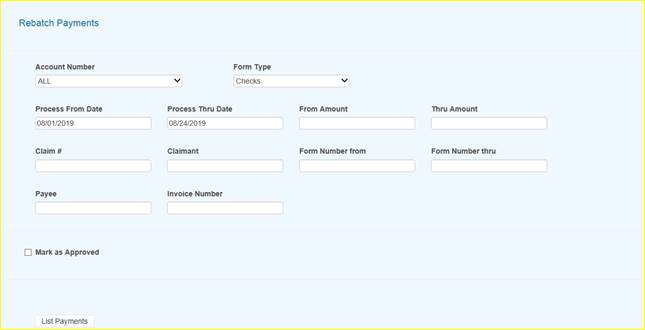
Figure 6‑9: Rebatch Payments Screen