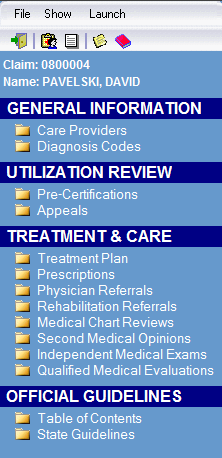
Case Management

Store information about the on-going medical treatment associated with a claim. This information includes the treating physician(s), diagnosis, treatment plan, prescriptions, appeals, referrals, reviews, second opinions, and independent examinations.
The Treatment Plan allows users to document information pertinent to the case. And, the timestamp feature can be used to maintain a chronological history and identify the user that made each entry.
The Pre-Certification screen allows users to document the Utilization Review process for requested procedures and produce standardized forms/letters that comply with State requirements, such as approval and/or denial letters.
An integrated browser provides direct access, via the web, to the Official Disability Guidelines (ODG) information about each Diagnosis Code, to assist with the Utilization Review process.
Users without Case Management rights have restricted access and can only enter information about Care Providers and Diagnosis Codes.
Fully equiped with correspondence and time billing features for a complete solution.